What Is OCD? Understanding Obsessive-Compulsive Disorder
Understanding Obsessive-Compulsive Disorder Beyond the Stereotypes
Obsessive-compulsive disorder (OCD) is often misunderstood. You might hear someone say "I'm so OCD" about liking things organized, but obsessive-compulsive disorder is a serious mental health condition that goes far beyond preferences for neatness. It's a mental disorder that causes unwanted thoughts and repetitive behaviors that can consume hours of your day and significantly interfere with work, relationships, or daily life.
If you're in Providence, Cranston, or elsewhere in Rhode Island and wondering what is OCD, this guide will help you understand the real symptoms, causes, and treatment options.
What Is Obsessive-Compulsive Disorder (OCD)?
Obsessive-compulsive disorder (OCD) is a chronic mental health condition characterized by obsessions and compulsions. These aren't just worries or habits—they're persistent, distressing experiences that consume significant time and cause substantial distress.
OCD affects about 1% to 3% of people in the United States. It typically starts in childhood, the teen years, or early adulthood, though it can develop at any age. Both men and women experience OCD at similar rates.
The symptoms often persist for years without appropriate treatment, but many people improve significantly with evidence-based care. People with obsessive-compulsive disorder OCD aren't just "particular" or "perfectionistic"—they experience genuine psychological distress from intrusive thoughts and feel compelled to perform rituals to manage overwhelming anxiety.
In our years working with clients who have OCD, we consistently see people who've been suffering in silence for a long time before seeking help. Many tell us they thought everyone had these kinds of thoughts, or that they should just be able to "get over it." What we want people in Rhode Island to know is that OCD is a real mental health condition, not a personality quirk or lack of willpower. The relief people feel when they finally understand what they're experiencing—and that effective treatment exists—is profound.
Understanding Obsessions
Obsessions are unwanted thoughts, mental images, or urges that repeatedly enter your mind and feel impossible to control. These obsessive thoughts are intrusive and distressing. They're also called obsessions because they involve repetitive behaviors of the mind—obsessional thinking that loops endlessly despite your efforts to stop it.
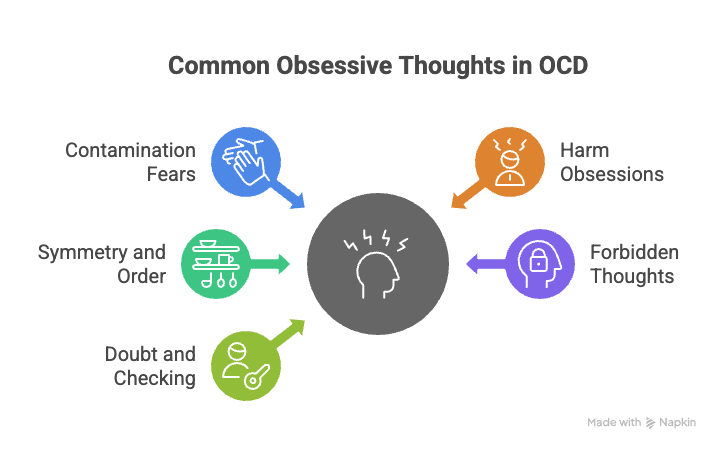
Common themes include:
Contamination fears - Intense worry about germs, dirt, or perceived contaminated substances
Harm obsessions - Unwanted thoughts about accidentally or intentionally hurting yourself or others
Symmetry and order - Overwhelming need for things to be arranged in a specific way
Forbidden thoughts - Disturbing mental images related to sexual, religious, or violent themes that cause unpleasant thoughts the person doesn't want
Doubt and checking - Persistent uncertainty about whether you completed important tasks
These obsessive fears aren't fleeting concerns. They're recurrent thoughts that cause significant anxiety and feel completely out of your control, even when you recognize they don't make logical sense.
Understanding Compulsions
Compulsions, also called compulsive behaviors or compulsive rituals, are repetitive behaviors or mental acts you feel driven to perform in response to obsessions. These aren't enjoyable activities—they're time-consuming actions you feel you must complete to reduce anxiety or prevent something terrible from happening. Compulsions can be observable ritualistic behaviors or internal mental acts like counting or praying silently.
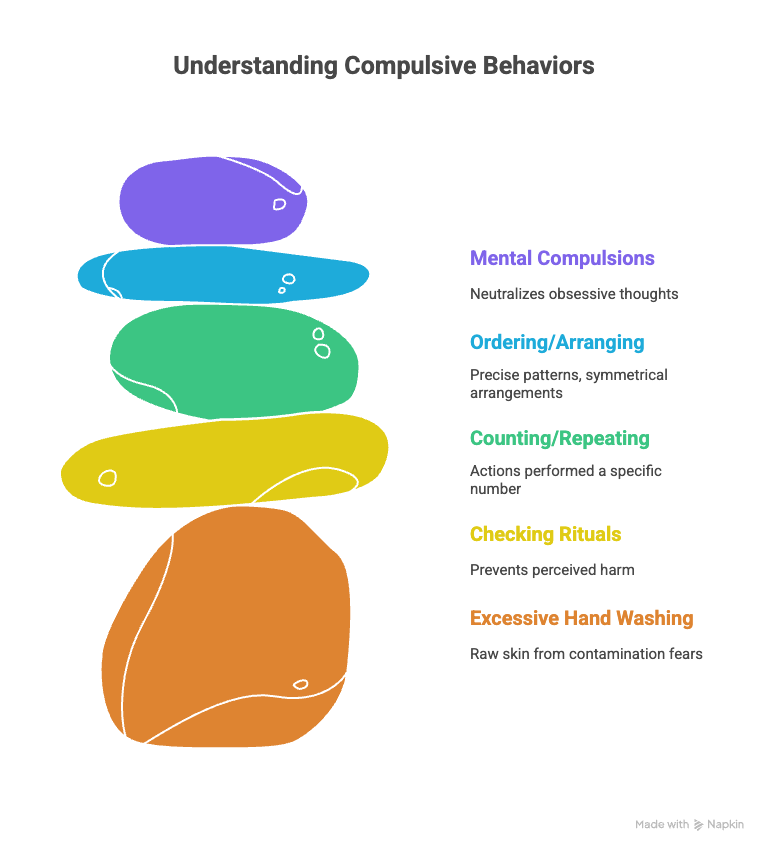
Common examples include:
Excessive hand washing - Washing hands repeatedly, sometimes until skin is raw, due to contamination fears
Checking rituals - Repeatedly checking locks, appliances, or switches to prevent harm
Counting or repeating - Performing actions a specific number of times or repeating words silently
Ordering and arranging - Organizing items in precise patterns or symmetrical arrangements
Mental compulsions - Silently praying, counting, or reviewing events to neutralize obsessive thoughts
People with OCD realize these compulsive behaviors are excessive, but the anxiety from not performing them feels unbearable. The temporary relief they provide reinforces the cycle, making obsessive-compulsive disorder OCD progressively more difficult to manage without treatment.
What Are 5 Symptoms of OCD?
The symptoms of OCD vary widely, but five key signs indicate someone may have this mental health condition:
Intrusive thoughts that won't stop - Unwanted thoughts, mental images, or urges that keep returning despite efforts to ignore or suppress them
Repetitive behaviors you can't resist - Feeling compelled to perform certain actions over and over, even when you know they're excessive
Time-consuming rituals - Spending more than an hour daily on obsessions and compulsions, often much longer
Significant distress or impairment - OCD symptoms interfere with work, school, relationships, or daily activities
Temporary relief followed by return of anxiety - Compulsions provide brief relief from anxiety, but obsessive thoughts return, perpetuating the cycle
Here's why this matters: OCD is diagnosed when obsessions and compulsions are time-consuming, cause distress, or significantly interfere with daily functioning. Many people experience occasional intrusive thoughts or prefer certain routines, but OCD represents a different level of impairment.
How to Tell If Someone Has OCD
Recognizing OCD in yourself or others requires looking beyond surface behaviors to understand the distress and compulsion driving them. People with obsessive-compulsive disorder often hide their symptoms due to embarrassment or shame, making it harder to identify.
Signs someone might have OCD include:
Spending excessive time on routine tasks (showering for hours, taking extremely long to leave the house)
Avoiding certain situations or objects that trigger obsessions
Repeatedly seeking reassurance from family members about their fears
Showing visible distress when unable to complete rituals
Having raw or damaged skin from excessive hand washing or cleaning
Difficulty concentrating due to intrusive thoughts
Withdrawing from social activities due to OCD symptoms
To diagnose OCD, a mental health professional will conduct a thorough assessment of thoughts, feelings, and behaviors. They may use standardized questionnaires and will evaluate whether symptoms meet criteria from the Diagnostic and Statistical Manual of Mental Disorders.
The key factors are whether obsessions and compulsions take up more than an hour daily, cause significant distress, or interfere with functioning.
It's worth noting that OCD often coexists with other mental health conditions. Anxiety disorders, depression, eating disorders, and substance abuse commonly occur alongside obsessive-compulsive disorder OCD. Understanding how to diagnose OCD and differentiate it from other mental disorders is important because treatment approaches can vary. Some people also experience related disorders like body dysmorphic disorder (excessive concern about perceived flaws in physical appearance), hoarding disorder (difficulty discarding possessions), skin picking (excoriation disorder), or hair pulling (trichotillomania).
What Causes OCD?
The exact causes of obsessive-compulsive disorder remain unknown, but research points to a combination of genetic, neurobiological, and environmental factors.
OCD tends to run in families, suggesting genetic vulnerability. Having a family history of OCD or other mental health disorders increases risk. However, family history alone doesn't determine who will develop OCD—many people with affected relatives never develop the condition.
Brain imaging studies reveal differences in brain circuits involved in decision-making, doubt, and habit formation. Some theories suggest OCD involves dysregulation of serotonin or other neurotransmitters, though the brain mechanisms are complex.
Environmental factors can trigger obsessions or compulsions in vulnerable individuals. Stressful life events, childhood trauma, or significant changes may precipitate OCD onset. In pediatric OCD, some cases are associated with streptococcal infections, a condition called pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS). Research studies continue to investigate this connection, though the relationship between streptococcal infections and sudden onset OCD symptoms in children remains an active area of study.
Here's what's crucial to understand: OCD is not caused by personal weakness or moral failing. It's not anyone's fault, and it's not caused by something you did or didn't do. It's a legitimate mental disorder requiring professional treatment.
What's It Like Living with OCD?
Living with obsessive-compulsive disorder can be exhausting and isolating. People with OCD may spend hours each day on obsessions and compulsions, leaving little time or energy for work, relationships, or activities they once enjoyed.
The experience varies depending on symptom severity. Some people with moderate symptoms can maintain jobs and relationships while struggling privately. Others with severe OCD find daily functioning nearly impossible—they may be unable to leave home, maintain employment, or care for themselves independently.
Common daily challenges include:
Taking hours to complete basic tasks like showering, getting dressed, or leaving the house
Missing work or school due to time spent on compulsive rituals
Avoiding social situations that might trigger obsessions
Straining relationships with family members who don't understand the compulsions
Feeling embarrassed, ashamed, or alone due to intrusive thoughts
Experiencing intense anxiety when prevented from completing rituals
Many people with OCD recognize their obsessive thoughts don't make sense and their compulsive behaviors are excessive. This awareness doesn't reduce the anxiety or the compulsion to perform rituals—in fact, it often adds to the distress. Understanding that your thoughts are irrational but being unable to stop them creates a frustrating disconnect.
We often tell clients in our practice that one of the hardest parts of OCD is this exact experience—knowing logically that checking the door twelve times doesn't make sense, but feeling physically unable to stop. The shame that comes with this disconnect keeps many people from reaching out for help. We want to be clear: This isn't about logic or willpower. OCD hijacks your anxiety system, and that's exactly why specialized treatment like ERP is so effective. You can't think your way out of OCD, but you can learn new responses that actually work.
The impact extends beyond the individual. Family members often become involved in rituals, either participating to help reduce a loved one's distress or avoiding behaviors that might trigger obsessions. This accommodation, while well-intentioned, can actually reinforce OCD symptoms over time.
How to Explain OCD to Someone
When explaining obsessive-compulsive disorder to someone unfamiliar with the condition, focus on the difference between preferences and compulsions.
You might say: "OCD isn't about liking things clean or organized. It's when unwanted thoughts create such intense anxiety that you feel forced to perform certain actions to make the anxiety stop—even when you know the actions don't make sense. Imagine being terrified something terrible will happen unless you wash your hands exactly 47 times, or that you've accidentally hurt someone unless you check the door 20 times before leaving. The anxiety is so overwhelming that resisting the compulsion feels impossible."
Key points to emphasize:
OCD involves genuine distress, not personality quirks
Compulsions aren't choices or preferences—they're driven by unbearable anxiety
People with OCD usually recognize their thoughts and behaviors are excessive
The condition significantly interferes with daily life
OCD is treatable with appropriate therapy and sometimes medication
It's helpful to explain that telling someone with OCD to "just stop" their compulsions is like telling someone with a broken leg to "just walk normally." The issue isn't lack of willpower—it's a mental health condition that requires proper treatment.
How Is OCD Treated?
The good news is that obsessive-compulsive disorder is highly treatable. The first-line treatment for OCD combines specific forms of therapy, and sometimes medication, based on symptom severity and individual needs.
Cognitive Behavioral Therapy and ERP
The most effective psychological treatment for OCD is cognitive behavioral therapy, specifically a technique called exposure and response prevention (ERP). Cognitive Behavioral Therapy (CBT) and ERP are considered the first line treatments for OCD because of its strong evidence base. This specialized form of cognitive therapy helps you gradually face situations that trigger obsessions while learning to resist performing compulsions.
In ERP, you work with a mental health professional to create a hierarchy of feared situations, ranking them from least to most anxiety-provoking. Then you gradually expose yourself to these situations, starting with less distressing ones, and practice tolerating the anxiety without performing compulsive rituals.
Here's an example: Someone with contamination fears might start by touching a doorknob and waiting 10 minutes before washing hands. They gradually build up to longer periods and more challenging exposures. The process teaches your brain that feared consequences don't actually occur and that anxiety subsides naturally without compulsions.
ERP can be done in individual therapy sessions, group settings, or intensive programs for severe symptoms. Many people show significant improvement with consistent ERP practice, though it requires commitment and can feel uncomfortable initially.
We approach ERP with this framework: discomfort in the service of freedom. The exposure exercises aren't meant to be easy—they're designed to help you build tolerance for anxiety without relying on compulsions. What we see in our work is that clients who push through the initial discomfort discover something powerful: the anxiety does decrease on its own, without rituals. That realization—that you can survive the anxiety and it will pass—changes everything. It's not about eliminating anxiety completely; it's about breaking the cycle that keeps OCD in control.
Medication for OCD
Selective serotonin reuptake inhibitors (SSRIs) are most commonly prescribed to treat OCD. These are the same class of antidepressants used for depression and anxiety disorders, but treating OCD typically requires higher doses and longer trial periods.
Common SSRIs include fluoxetine, sertraline, paroxetine, and fluvoxamine. These medications may take 8-12 weeks at adequate doses to show benefit for OCD symptoms, longer than the 4-6 weeks typical for depression.
Medication alone is often less effective than therapy alone or combined treatment. Many people benefit from combining ERP with SSRIs, especially for moderate to severe symptoms. The medication can reduce symptom intensity enough to make engaging in exposure exercises more manageable.
Advanced Treatment Options
For treatment-resistant OCD that doesn't respond to standard approaches, other options exist. Treatment-resistant OCD refers to cases where symptoms don't improve adequately after appropriate trials of both ERP and medication:
Augmentation strategies - Adding a second medication, sometimes from the antipsychotic class, to enhance SSRI effectiveness
Intensive outpatient or residential programs - More frequent therapy sessions for severe OCD symptoms
Deep brain stimulation - A surgical procedure approved for severe, treatment-resistant cases
Transcranial magnetic stimulation - A non-invasive brain stimulation technique showing promise in research studies
These advanced interventions are typically considered only after thorough trials of ERP and medication haven't produced adequate improvement.
Other Supportive Approaches
While not replacements for evidence-based treatment to treat OCD, some people find these helpful as supplements:
Support groups - Connecting with others who understand the challenges of OCD can reduce isolation
Stress management - Relaxation techniques, mindfulness, or exercise to help manage overall anxiety
Family therapy - Helping family members understand OCD and learn how to support appropriate treatment without accommodating symptoms
Talk therapy - General counseling can address the emotional impact and relationship difficulties caused by living with this mental health condition
Related Mental Health Conditions
OCD is classified alongside several related disorders that share similar features. Understanding these connections helps recognize the broader category of obsessive-compulsive and related disorders:
Body dysmorphic disorder involves obsessive thoughts about perceived flaws in physical appearance and compulsive behaviors like mirror checking or excessive grooming. The obsessional thinking patterns mirror OCD, focused specifically on appearance concerns.
Hoarding disorder is characterized by persistent difficulty discarding possessions, regardless of actual value, leading to cluttered living spaces that interfere with use of home areas. While once considered a type of OCD, it's now classified as a related disorder with distinct features.
Hair pulling (trichotillomania) and skin picking (excoriation disorder) involve repetitive behaviors that result in noticeable damage. These body-focused repetitive behaviors share some features with compulsive rituals but have important differences in treatment approach.
Tic disorders, including Tourette syndrome, frequently co-occur with OCD. Tics are sudden, rapid, recurrent movements or vocalizations, distinct from compulsive behaviors but sometimes overlapping in pediatric OCD.
Understanding these related disorders matters because they may require modifications to standard OCD treatment approaches. A mental health professional can evaluate whether symptoms fit OCD criteria or represent a related condition requiring different intervention.
Finding Help for OCD in Rhode Island
If you think you might have obsessive-compulsive disorder, reaching out to a mental health professional is the important first step. Early intervention can prevent symptoms from worsening and improve long-term outcomes. Mental health professionals can properly diagnose OCD and determine how it should be treated based on your specific symptoms and needs.
In Rhode Island, start by talking with your primary care doctor about your concerns. They can provide referrals to mental health professionals who specialize in treating OCD using evidence-based approaches like ERP.
OCD is a chronic condition, but it's highly treatable. Many people experience substantial improvement with appropriate treatment. Some achieve full remission, while others learn to manage symptoms effectively even if they occasionally recur during stressful periods.
The key is finding a mental health professional trained in evidence-based OCD treatment and committing to the process, even when exposure exercises feel uncomfortable. Recovery takes time, but it's absolutely possible.
If you're looking for support with OCD in Rhode Island, the therapists at Providence Therapy Group are here to help. Schedule an appointment to get started.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.